Optimizing your revenue impact, risk scores and error rates
Where health insurance professionals converge to enhance risk management, share analytical insights, foster collaboration, and explore cutting-edge solutions to tackle challenges in risk adjustment and leverage analytics for better decision-making and cost control.
This event will bring together:
- Insurers
- Data Vendors

Optimizing Your Accounts Receivable Strategies
Where healthcare leaders gather to maximize revenue, exchange best practices, foster collaboration, and explore innovative solutions.
This event will bring together:
- Hospitals
- Healthcare Systems
- Physician Networks
- Clinical Practices
- Patient Access Vendors
- Accounts Receivable Management Vendors
- Medical Billing Vendors
- Denial Management Vendors

Optimizing Your Claims Management
Where healthcare leaders come to increase savings, share strategies, foster collaboration and discover innovative solutions to tackle challenges along the claims continuum and identify cost containment opportunities.
This event will bring together:
- Insurers
- Healthcare Providers
- PI Vendors
- FWA Vendors
- AI Healthcare Vendors
Speaker Faculty Includes:

Bruce Lim
Bruce Lim serves as the Deputy Director, Audits and Investigations, for the California Department of Health Care Services (DHCS) and is the designated Program Integrity Director for Medi-Cal, California’s Medicaid program. Mr. Lim is a certified public accountant (CPA) with over 32 years of audit and financial management experience in both the private and public sectors. Past employers include Kenneth Leventhal and Company, CPAs (Ernst & Young Kenneth Leventhal Real Estate Group), Packard Bell NEC, and the California Department of Food and Agriculture.

Christopher Draven
Christopher Draven is Senior Director of Payment Integrity Analytics & AI at HCSC where he leads a cross-functional team focused on delivering actionable insights and savings. He has over 25 years experience in healthcare, starting in direct patient care.

Kelly Bennett, JD, CFE, AHFI
Kelly Bennett graduated from the University of Tampa and Florida State University College of Law. She has been a member of the Florida Bar since 1997 and is a Certified Fraud Examiner and an Accredited Health Care Fraud Investigator. She has worked at the Florida Agency for Health Care Administration since 2001 and has served in several roles, including as a Senior Attorney within the Medicaid Division of the Office of the General Counsel, the Assistant Bureau Chief for the Bureau of Medicaid Program Integrity, the Agency’s Medicaid
Fraud Liaison, and is currently the Chief of Medicaid Program Integrity, where she has served since July of 2014. She is currently the President for the National Association for Medicaid Program Integrity and is an active participant in training and collaboration initiatives with the National Health Care Antifraud Association.

Cynthia Johnson

Andrew Zurick

Becky Peters

Dr Priscilla Alfaro, MD, FAAP, CPC, CPMA, COC, CIC, CFE
Dr. Priscilla Alfaro is a seasoned healthcare professional with extensive experience in executive medical management, fraud prevention, and healthcare analytics. A certified medical coder, fraud examiner, and auditor, she has a proven track record of improving healthcare efficiency and preventing fraud, waste, and abuse across various roles and affiliations, including the Texas HHS and Anthem.

Monique Pierce
Monique is a Strategic Executive Healthcare Leader with proven ability to develop solutions and maximize the benefits of Payment Integrity programs. She is known for having excellent domain knowledge and being driven, high performing, and having a deep dedication to recruiting and developing top talent.
Monique started her Payment Integrity career at Oxford HealthPlans in the COB and Subrogation Department after spending time in Payment Policy. When United Healthcare acquired many health plans in the early 2000s like Oxford, Monique was tagged as part of the Optum team to integrate the processes and people into the COB systems that she had built at Oxford. She led systems development, quality, reporting, operations, vendor management and was responsible for creating innovative proactive programs that more than doubled savings to $1.4B in three years.
Monique developed a successful program that reduced interest expense on late claims for UHC, assisted a communication company to develop COB tools and assisted in strategic system projects before joining SCIO Health Analytics in 2014 to develop new products - specifically prepayment programs.
In 2015 she became the product owner of SCIOMine, the company’s internal audit application and managed the roadmap. Monique also owned
strategic direction for operational metrics and reporting including executive scorecards. Monique was promoted to VP of Business Opportunities and Client Engagement where she improved Audit Recovery TAT by 39% and reduced client implementations TAT by 11% and the Level of Effort by 18% while increasing the count of implementation projects by 126%.
In 2020 Monique joined Devoted Health, a startup company with the goal of building the first ever integrated Payment Integrity Program. The company has one system, great data, and a great mission; to change health care by treating every member as if they are family.
In her spare time, Monique volunteers her time in the community on the Board of Directors of SCARE NH and works in her family business LARP Portal with her husband Rick.

Frank Shipp
Frank E. Shipp currently serves as Executive Director of the Johns Hopkins Clinical Alliance, the clinically integrated network of Johns Hopkins Medicine. The network includes over 3,000 providers, consisting of both employed and independent practices.
Frank transitioned to value-based care after 25 years of hospital-based operations experience in both community and academic health systems. During the past nine years, Frank has held executive positions in a Payor-Provider Organization in NYC and has built a highly successful CIN over a five-year period in Northern New Jersey. Frank speaks regular at national healthcare conferences regarding value-based care strategies and tactics.
Frank completed his MBA at Fairleigh Dickinson University, is a certified Fellow of the American College of Healthcare Executives and a trained Black Belt in Lean Six Sigma from Villanova University.

Corella Lumpkins
Corella Lumpkins is the Manager of Coding, Compliance & Provider Education at Loudoun Medical Group (LMG) - one of the largest and most diverse physician-owned, multi-specialty Accountable Care Organizations in Northern Virginia/DC suburbs. As a subject matter expert, Corella has over 35 years of experience working in every area of the healthcare revenue cycle. Corella holds a bachelor’s degree and eleven certifications with an extensive background in auditing, billing, coding, implementing corporate compliance programs, CDI, education, denial and practice management. Prior to joining LMG, Corella has held leadership roles at Lifebridge, Medstar, Johns Hopkins and the University of Maryland health systems.
Corella is an author, adjunct faculty member and national speaker currently serving on both the AAPC National Advisory Board and Association of Clinical Documentation Integrity Specialists (ACDIS) Leadership Council. Corella works closely with providers in navigating patient-centric value-based care.

Helen Liu, Pharm.D.
Dr. Liu is the Vice President of Pharmacy Operations for the ATRIO Health Plans, where she manages and oversees all Part D-related operations. Dr Liu has an extensive background in clinical pharmacy, medication safety, managed care, and data outcome analysis. Before this role, she developed and implemented the inpatient Drug Use Management program at Kaiser Permanente.

Jordan Limperis
Highly motivated Data Scientist with a strong background in healthcare data and systems. Experienced in Inpatient Hospital and Laboratory Epic Systems, where I applied data-driven insights to improve clinical and operational efficiency. Currently, I am pursuing my career at L.A. Care, focusing leveraging advanced machine learning techniques to analyze noisy data, ensuring accuracy and efficiency in healthcare operations, particularly in payment integrity.
Your go-to for everything Healthcare

Bigger, better audience
With now 3 separate curated topics, we aim to unite payers and providers across everything finance. Covering the liked of payment integrity and risk adjustment from the health plan side and revenue cycle management on the provider side, we include all aspects of payer-provider collaboration across healthcare finance.

Facilitated Networking
We’re helping you keep up to date with solutions on the market and curating the conversations you have with vendors so you meet those who can really help your organizations save more. Expect trailblazing solutions in payment integrity, risk adjustment and revenue cycle management.
HEAR FROM OUR AUDIENCE

It's a unique forum that brings together providers, payors, vendors and regulators for collaboration, education and information sharing.

It was a seamless process and the intimate meeting space was ideal to allow for more collaboration

The quality of the event, sessions, speakers and Health Plan attendees scored high

Great job putting on your inaugural show. I'm certain that the show will continue to grow and get even better in the future.

I think the conference has good potential going forward. It fits a niche in the industry.

This conference filled the much needed gap in focusing on Payment Integrity issues and initiatives

We finally have a PI conference!

This PI conference was wonderful. We’d rank it 10/10 with representation from all across the industry

This was the most meaningful industry event of the year for Payment Integrity professionals

It was a great opportunity to hear from many subject matter experts over a wide topic of subjects specific to Payment/Revenue Integrity
OUR COMMUNITY OF PAYERS AND PROVIDERS

Demonstrate your tech and leadership by partnering with us
Partner with us to elevate your brand, and make valuable new connections. Subject to availability, we offer opportunities for thought leadership, branding, and facilitated networking.
Please contact our Partnerships Director, Harry Ludbrook, for more information. [email protected].

Healthcare Payers and Providers attend for free
Step into interactive discussions and engaging presentations on the key challenges and opportunities presented by payment companies.
If you are from a healthcare plan or provider organization, you can join our events for free.
TELL ME MORE
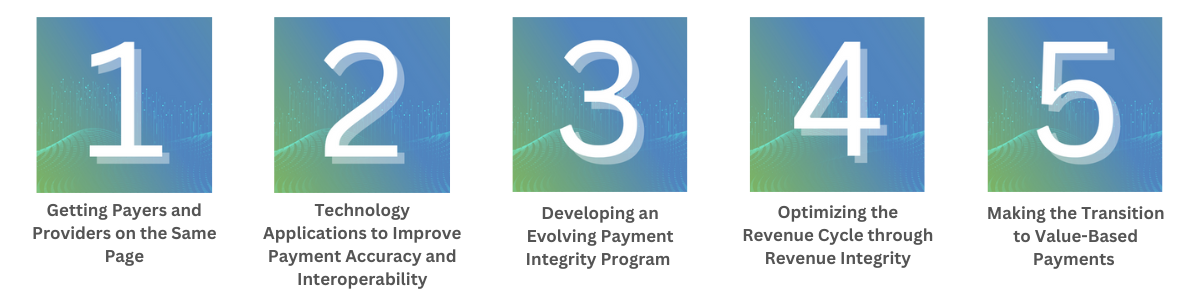
The 2nd Annual Healthcare Payment and Revenue Integrity Congress East, is an opportunity for leaders in PI and RI/RCM to come together and discuss emerging solutions to prominent issues including improving audits, resource prioritization, adjusting to new trends in healthcare demands and policy, and improving payer-provider relationships.
As a health plan, this congress will give you the resources to strengthen, redefine, or establish your own payment integrity strategies by analyzing case studies from industry peers and joining interactive discussions that span the entire claims continuum.
As a revenue cycle management expert, you can evaluate the use of intelligent automation and AI within your organisation to optimize revenue integrity, while also getting to address chargemaster integrity, understand value-based payment models and establishing strong cross functional collaboration on coding, billing, compliance and beyond.

Highlights:
The Payment Integrity Vendor Landscape
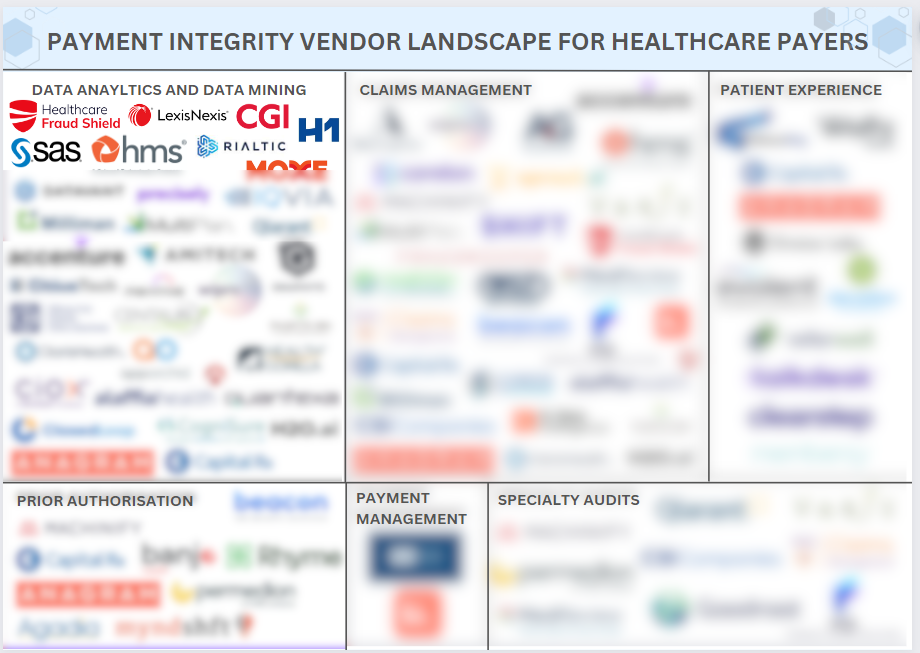
Navigating the Payment Integrity Vendor landscape can be daunting for health plans and providers, given the multitude of vendors and their diverse specialties. With so many options available, it's often difficult to identify the best partners. That's why we've created this document, which showcases the top vendors tailored to your specific needs including:
- Fraud Anayltics
- Provider Networking/Contracting
- PI BPO
- Pharmacy Benefit Management
- Coordination of Benefits
- Subrogration
- Risk Adjustment/Analytics
- Data Analytics and Data Mining
- Claims Management
- Patient Experience
- Specialty Audits
- Prior Authorisation
- Payment Management
Welcome to the 2nd Annual HPRI Congress East!
The Healthcare Payment and Revenue Integrity Congress connects leading figures in PI and RI/RCM to encourage information sharing, discuss the latest solutions being leveraged to ensure the integrity of claims, nurture payer-providers relationships and support the transition to value-based payments.
Health plans use this forum to strengthen, redefine, or establish their own payment integrity strategies by analyzing case studies from industry peers and joining interactive discussions that span the entire claims continuum.
It also empowers providers to make revenue cycle decisions with confidence by leveraging intelligent automation, optimizing RCM based on value, and effectively communicating concerns around emerging payment initiatives.
Would you like to present at the upcoming event?
Showcase your work to our audience of 150+ payment integrity leaders.
If you would be interested in learning about the speaking opportunities available, please email [email protected]
Photo Gallery
HOW TO GET INVOLVED

Partner With Us
Partner with us to elevate your brand, and make valuable new connections. Subject to availability, we offer opportunities for thought leadership, branding, and facilitated networking.
Please contact our Partnerships Director, Harry Ludbrook, for more info.

Payers And Providers Attend For Free
Step into interactive discussions and engaging presentations on the key challenges and opportunities presented by payment companies.
To deliver maximum value for our community, all payers and providers are eligible for complimentary passes.
OUR COMMUNITY

FEATURED SPEAKERS

Bruce Lim
Bruce Lim serves as the Deputy Director, Audits and Investigations, for the California Department of Health Care Services (DHCS) and is the designated Program Integrity Director for Medi-Cal, California’s Medicaid program. Mr. Lim is a certified public accountant (CPA) with over 32 years of audit and financial management experience in both the private and public sectors. Past employers include Kenneth Leventhal and Company, CPAs (Ernst & Young Kenneth Leventhal Real Estate Group), Packard Bell NEC, and the California Department of Food and Agriculture.

Christopher Draven
Christopher Draven is Senior Director of Payment Integrity Analytics & AI at HCSC where he leads a cross-functional team focused on delivering actionable insights and savings. He has over 25 years experience in healthcare, starting in direct patient care.

Crystal Son
Crystal Son is an Executive Director of Enterprise Data Analytics Solutions at Healthcare Service Corporation (HCSC). She has 19 years of experience in deriving intelligence from data.
At HCSC, she leads the Strategic Initiatives & Partnerships team, a department that focuses on cross-functional, collaborative analytics delivery on key programs such as Payment Integrity and Stakeholder Engagement, enterprise data and analytics strategy and planning, as well as design and execution of HCSC’s Responsible AI program. She is passionate about real-world applications of data-driven insights, storytelling through data, and building high-performance teams.

Helen Liu, Pharm.D.
Dr. Liu is the Vice President of Pharmacy Operations for the ATRIO Health Plans, where she manages and oversees all Part D-related operations. Dr Liu has an extensive background in clinical pharmacy, medication safety, managed care, and data outcome analysis. Before this role, she developed and implemented the inpatient Drug Use Management program at Kaiser Permanente.

Kelly Bennett, JD, CFE, AHFI
Kelly Bennett graduated from the University of Tampa and Florida State University College of Law. She has been a member of the Florida Bar since 1997 and is a Certified Fraud Examiner and an Accredited Health Care Fraud Investigator. She has worked at the Florida Agency for Health Care Administration since 2001 and has served in several roles, including as a Senior Attorney within the Medicaid Division of the Office of the General Counsel, the Assistant Bureau Chief for the Bureau of Medicaid Program Integrity, the Agency’s Medicaid
Fraud Liaison, and is currently the Chief of Medicaid Program Integrity, where she has served since July of 2014. She is currently the President for the National Association for Medicaid Program Integrity and is an active participant in training and collaboration initiatives with the National Health Care Antifraud Association.

Cynthia Johnson
AGENDA HIGHLIGHTS
CMS Center for Program Integrity (CPI) Updates
- This session will be focused on providing an insider’s view of CPI and CPI’s 2023 priorities
- We will cover the use of the Government Accountability Office Fraud Risk Management Framework to develop anti-fraud strategies and react to emerging threats, updates on our Marketplace fraud work, and opportunities for private-public collaboration.

Jennifer Dupee
Jennifer Dupee, Director. Audits & Vulnerabilities Group. Center for Program Integrity
In her role as the Director of the Audits and Vulnerabilities Group, Ms. Dupee identifies and develops comprehensive mitigation strategies addressing program integrity risks for all of CMS' programs, provides oversight of Medicare Part C and Part D plans and the Federally Facilitated Exchanges, and implements CMS’ Comprehensive Medicaid Integrity Plan. Prior to her current role at CPI, Ms. Dupee worked on such initiatives as the improper payment rate measurement for the Medicare fee-for-service program, Open Payments, and the Healthcare Fraud Prevention Partnership. Ms. Dupee also completed a Congressional detail with the House Committee on Ways and Means, responsible for a portfolio of Medicare fee-for-service and program integrity issues. Ms. Dupee has a Bachelor of Science Degree in Nursing from the University of Wisconsin, a Master of Science in Nursing and a Master of Business Administration from Johns Hopkins University, and a Juris Doctor Degree with a Health Law Certificate from the University of Maryland.
Developing A Payment Integrity Program From The Ground Up
- Developing a Payment Integrity Program from the ground up for a brand new Medicare Advantage Health Plan
- Covering both the opportunities and the challenges of building and effectively managing PI programs that prevent, avoid, or recover billing errors, payment errors and other party liability errors
- Listing of suggestions/ advice from our success, and lessons learned

Monique Pierce
Monique is a Strategic Executive Healthcare Leader with proven ability to develop solutions and maximize the benefits of Payment Integrity programs. She is known for having excellent domain knowledge and being driven, high performing, and having a deep dedication to recruiting and developing top talent.
Monique started her Payment Integrity career at Oxford HealthPlans in the COB and Subrogation Department after spending time in Payment Policy. When United Healthcare acquired many health plans in the early 2000s like Oxford, Monique was tagged as part of the Optum team to integrate the processes and people into the COB systems that she had built at Oxford. She led systems development, quality, reporting, operations, vendor management and was responsible for creating innovative proactive programs that more than doubled savings to $1.4B in three years.
Monique developed a successful program that reduced interest expense on late claims for UHC, assisted a communication company to develop COB tools and assisted in strategic system projects before joining SCIO Health Analytics in 2014 to develop new products - specifically prepayment programs.
In 2015 she became the product owner of SCIOMine, the company’s internal audit application and managed the roadmap. Monique also owned
strategic direction for operational metrics and reporting including executive scorecards. Monique was promoted to VP of Business Opportunities and Client Engagement where she improved Audit Recovery TAT by 39% and reduced client implementations TAT by 11% and the Level of Effort by 18% while increasing the count of implementation projects by 126%.
In 2020 Monique joined Devoted Health, a startup company with the goal of building the first ever integrated Payment Integrity Program. The company has one system, great data, and a great mission; to change health care by treating every member as if they are family.
In her spare time, Monique volunteers her time in the community on the Board of Directors of SCARE NH and works in her family business LARP Portal with her husband Rick.
Claims Audit – The Indiana Jones of Payment Integrity?
- How does Claim Audit fit into the overall savings goals from PI?
- Archaeology amongst savings drivers? High $ treasures?
- Claim Audit Digs & Research – driving process improvement, not just savings.
- Do underpayments matter?
- How to keep finding treasure:
- Partnering with other departments as a true “Partner” not an “Auditor.”
- It will all be in a museum (creating reference materials).

Tom Martin
Step into interactive discussions and engaging presentations on the key challenges and opportunities presented by payment companies today:
OUR PARTNERS

OUR SELECTION COMITTEE

Brannon Morisoli
Mr. Morisoli joined SWK Holdings as a Senior Analyst in March 2016. Prior to joining SWK, he was an Investment Analyst and Portfolio Manager for a family office that invested in equities, fixed income, real estate, and alternative investments. Prior to that, he was an Investment Analyst for Presidium Group, a real estate private equity firm, where he played an integral role in closing over $100mm in transactions. Mr. Morisoli began his career at Neurografix, a startup medical technology company in Santa Monica, CA that was doing groundbreaking work in the MRI imaging of peripheral nerves. While with Neurografix, he was published in two leading neurology journals. Brannon graduated from UCLA with a B.S., was awarded a fellowship and graduated from the University of Notre Dame with an M.B.A, and was awarded a Samson Fellowship from the University of Wisconsin Law School, where he graduated with a J.D. Mr. Morisoli is an inactive member of the State Bar of Wisconsin

Thomas Busby
Thomas Busby is a Vice President and has been with Outcome Capital since 2015. He focuses on medical technology, digital health and life science services segments with particular interest in innovative life science companies that deliver patient impact by leveraging novel approaches. Thomas is driven by the desire to identify disruptive technologies and services that require unique strategic thought and assistance to realize their full market potential. Thomas has been published in leading life science journals Life Science Leader and The Pharma Letter, and also serves on the board of HealthTech Build, a Boston-based digital health innovation group.
Prior to his career in life-science investment banking, Thomas pursued his passion for the public service and non-profit sectors working in a variety of leadership and management positions, and at one time held a Massachusetts teaching license.
Thomas completed his MBA at Suffolk University’s Sawyer Business School on full academic scholarship where he was President of the school’s Graduate Business Association and class speaker at graduation. Prior, he completed a BS in Philosophy with Honors from Suffolk’s College of Arts & Sciences. Committed to giving back, Thomas is currently the President of the College of Arts & Sciences Alumni Board of Directors. Thomas is a FINRA Registered Securities Representative holding his Series 79 and 63.

Robert Crousore
Robert has 28 years of experience in the health care products and
services industry. Crousore is a serial entrepreneur with multiple
successful product and services company exits. His experience spans
the entire business enterprise including Sales, Marketing, Operations,
Product Innovation and, most recently M & A.
Highlights Include:
- Has successfully managed a global commercial organization in the wound care business.
- Has a number of patent credits for products in the wound care industry.
- Sits on multiple boards of healthcare technology companies.
- His passion is creating meaningful changes in patient care by combining great products with great teams that are focused on empowering improved clinical and financial outcomes.

Brannon Morisoli
Mr. Morisoli joined SWK Holdings as a Senior Analyst in March 2016. Prior to joining SWK, he was an Investment Analyst and Portfolio Manager for a family office that invested in equities, fixed income, real estate, and alternative investments. Prior to that, he was an Investment Analyst for Presidium Group, a real estate private equity firm, where he played an integral role in closing over $100mm in transactions. Mr. Morisoli began his career at Neurografix, a startup medical technology company in Santa Monica, CA that was doing groundbreaking work in the MRI imaging of peripheral nerves. While with Neurografix, he was published in two leading neurology journals. Brannon graduated from UCLA with a B.S., was awarded a fellowship and graduated from the University of Notre Dame with an M.B.A, and was awarded a Samson Fellowship from the University of Wisconsin Law School, where he graduated with a J.D. Mr. Morisoli is an inactive member of the State Bar of Wisconsin

Thomas Busby
Thomas Busby is a Vice President and has been with Outcome Capital since 2015. He focuses on medical technology, digital health and life science services segments with particular interest in innovative life science companies that deliver patient impact by leveraging novel approaches. Thomas is driven by the desire to identify disruptive technologies and services that require unique strategic thought and assistance to realize their full market potential. Thomas has been published in leading life science journals Life Science Leader and The Pharma Letter, and also serves on the board of HealthTech Build, a Boston-based digital health innovation group.
Prior to his career in life-science investment banking, Thomas pursued his passion for the public service and non-profit sectors working in a variety of leadership and management positions, and at one time held a Massachusetts teaching license.
Thomas completed his MBA at Suffolk University’s Sawyer Business School on full academic scholarship where he was President of the school’s Graduate Business Association and class speaker at graduation. Prior, he completed a BS in Philosophy with Honors from Suffolk’s College of Arts & Sciences. Committed to giving back, Thomas is currently the President of the College of Arts & Sciences Alumni Board of Directors. Thomas is a FINRA Registered Securities Representative holding his Series 79 and 63.

Robert Crousore
Robert has 28 years of experience in the health care products and
services industry. Crousore is a serial entrepreneur with multiple
successful product and services company exits. His experience spans
the entire business enterprise including Sales, Marketing, Operations,
Product Innovation and, most recently M & A.
Highlights Include:
- Has successfully managed a global commercial organization in the wound care business.
- Has a number of patent credits for products in the wound care industry.
- Sits on multiple boards of healthcare technology companies.
- His passion is creating meaningful changes in patient care by combining great products with great teams that are focused on empowering improved clinical and financial outcomes.
SPEAKERS

Bruce Lim
Bruce Lim serves as the Deputy Director, Audits and Investigations, for the California Department of Health Care Services (DHCS) and is the designated Program Integrity Director for Medi-Cal, California’s Medicaid program. Mr. Lim is a certified public accountant (CPA) with over 32 years of audit and financial management experience in both the private and public sectors. Past employers include Kenneth Leventhal and Company, CPAs (Ernst & Young Kenneth Leventhal Real Estate Group), Packard Bell NEC, and the California Department of Food and Agriculture.

Christopher Draven
Christopher Draven is Senior Director of Payment Integrity Analytics & AI at HCSC where he leads a cross-functional team focused on delivering actionable insights and savings. He has over 25 years experience in healthcare, starting in direct patient care.

Crystal Son
Crystal Son is an Executive Director of Enterprise Data Analytics Solutions at Healthcare Service Corporation (HCSC). She has 19 years of experience in deriving intelligence from data.
At HCSC, she leads the Strategic Initiatives & Partnerships team, a department that focuses on cross-functional, collaborative analytics delivery on key programs such as Payment Integrity and Stakeholder Engagement, enterprise data and analytics strategy and planning, as well as design and execution of HCSC’s Responsible AI program. She is passionate about real-world applications of data-driven insights, storytelling through data, and building high-performance teams.

Helen Liu, Pharm.D.
Dr. Liu is the Vice President of Pharmacy Operations for the ATRIO Health Plans, where she manages and oversees all Part D-related operations. Dr Liu has an extensive background in clinical pharmacy, medication safety, managed care, and data outcome analysis. Before this role, she developed and implemented the inpatient Drug Use Management program at Kaiser Permanente.

Kelly Bennett, JD, CFE, AHFI
Kelly Bennett graduated from the University of Tampa and Florida State University College of Law. She has been a member of the Florida Bar since 1997 and is a Certified Fraud Examiner and an Accredited Health Care Fraud Investigator. She has worked at the Florida Agency for Health Care Administration since 2001 and has served in several roles, including as a Senior Attorney within the Medicaid Division of the Office of the General Counsel, the Assistant Bureau Chief for the Bureau of Medicaid Program Integrity, the Agency’s Medicaid
Fraud Liaison, and is currently the Chief of Medicaid Program Integrity, where she has served since July of 2014. She is currently the President for the National Association for Medicaid Program Integrity and is an active participant in training and collaboration initiatives with the National Health Care Antifraud Association.

Cynthia Johnson

Andrew Zurick

Becky Peters

Betye Ochoa

Ebrahim Barkoudah

Jordan Limperis
Highly motivated Data Scientist with a strong background in healthcare data and systems. Experienced in Inpatient Hospital and Laboratory Epic Systems, where I applied data-driven insights to improve clinical and operational efficiency. Currently, I am pursuing my career at L.A. Care, focusing leveraging advanced machine learning techniques to analyze noisy data, ensuring accuracy and efficiency in healthcare operations, particularly in payment integrity.

Monique Pierce
Monique is a Strategic Executive Healthcare Leader with proven ability to develop solutions and maximize the benefits of Payment Integrity programs. She is known for having excellent domain knowledge and being driven, high performing, and having a deep dedication to recruiting and developing top talent.
Monique started her Payment Integrity career at Oxford HealthPlans in the COB and Subrogation Department after spending time in Payment Policy. When United Healthcare acquired many health plans in the early 2000s like Oxford, Monique was tagged as part of the Optum team to integrate the processes and people into the COB systems that she had built at Oxford. She led systems development, quality, reporting, operations, vendor management and was responsible for creating innovative proactive programs that more than doubled savings to $1.4B in three years.
Monique developed a successful program that reduced interest expense on late claims for UHC, assisted a communication company to develop COB tools and assisted in strategic system projects before joining SCIO Health Analytics in 2014 to develop new products - specifically prepayment programs.
In 2015 she became the product owner of SCIOMine, the company’s internal audit application and managed the roadmap. Monique also owned
strategic direction for operational metrics and reporting including executive scorecards. Monique was promoted to VP of Business Opportunities and Client Engagement where she improved Audit Recovery TAT by 39% and reduced client implementations TAT by 11% and the Level of Effort by 18% while increasing the count of implementation projects by 126%.
In 2020 Monique joined Devoted Health, a startup company with the goal of building the first ever integrated Payment Integrity Program. The company has one system, great data, and a great mission; to change health care by treating every member as if they are family.
In her spare time, Monique volunteers her time in the community on the Board of Directors of SCARE NH and works in her family business LARP Portal with her husband Rick.

Dr Priscilla Alfaro, MD, FAAP, CPC, CPMA, COC, CIC, CFE
Dr. Priscilla Alfaro is a seasoned healthcare professional with extensive experience in executive medical management, fraud prevention, and healthcare analytics. A certified medical coder, fraud examiner, and auditor, she has a proven track record of improving healthcare efficiency and preventing fraud, waste, and abuse across various roles and affiliations, including the Texas HHS and Anthem.

Simi Binning
Simi Binning is an accomplished healthcare professional with over a decade of experience in developing and executing successful strategies that drive business growth. Currently serving as a Responsible AI lead at HCSC, her focus is on AI governance and innovative problem solving.

Edward Thomas

Frank Shipp
Frank E. Shipp currently serves as Executive Director of the Johns Hopkins Clinical Alliance, the clinically integrated network of Johns Hopkins Medicine. The network includes over 3,000 providers, consisting of both employed and independent practices.
Frank transitioned to value-based care after 25 years of hospital-based operations experience in both community and academic health systems. During the past nine years, Frank has held executive positions in a Payor-Provider Organization in NYC and has built a highly successful CIN over a five-year period in Northern New Jersey. Frank speaks regular at national healthcare conferences regarding value-based care strategies and tactics.
Frank completed his MBA at Fairleigh Dickinson University, is a certified Fellow of the American College of Healthcare Executives and a trained Black Belt in Lean Six Sigma from Villanova University.

Garland Goins Jr

Jill Sell-Kruse

Corella Lumpkins
Corella Lumpkins is the Manager of Coding, Compliance & Provider Education at Loudoun Medical Group (LMG) - one of the largest and most diverse physician-owned, multi-specialty Accountable Care Organizations in Northern Virginia/DC suburbs. As a subject matter expert, Corella has over 35 years of experience working in every area of the healthcare revenue cycle. Corella holds a bachelor’s degree and eleven certifications with an extensive background in auditing, billing, coding, implementing corporate compliance programs, CDI, education, denial and practice management. Prior to joining LMG, Corella has held leadership roles at Lifebridge, Medstar, Johns Hopkins and the University of Maryland health systems.
Corella is an author, adjunct faculty member and national speaker currently serving on both the AAPC National Advisory Board and Association of Clinical Documentation Integrity Specialists (ACDIS) Leadership Council. Corella works closely with providers in navigating patient-centric value-based care.

Ankur Verma
Ankur Verma is a member of the Business Process Services team and assists clients on topics related to optimizing business process service delivery models, with an emphasis on Healthcare (payers and providers) and Life Sciences. Ankur’s responsibilities include assisting in managing Everest Group’s Healthcare and Life Sciences Outsourcing subscription offerings and providing outsourcing advisory services to clients on an ad hoc basis.
Prior to joining Everest Group, Ankur was a Senior Analyst with The Smartcube. He holds a bachelor’s degree in technology from Netaji Subhas Institute of Technology, Delhi.

Lisa Meredith

Paul LePage

Paul Schmitz

Richelle Marting, JD, MHSA,RHIA,CPC,CEMC,CPMA

Sandy Giangreco Brown

Willie Brown
AGENDA
CMS Center for Program Integrity (CPI) Updates
- This session will be focused on providing an insider’s view of CPI and CPI’s 2023 priorities
- We will cover the use of the Government Accountability Office Fraud Risk Management Framework to develop anti-fraud strategies and react to emerging threats, updates on our Marketplace fraud work, and opportunities for private-public collaboration.

Jennifer Dupee
Jennifer Dupee, Director. Audits & Vulnerabilities Group. Center for Program Integrity
In her role as the Director of the Audits and Vulnerabilities Group, Ms. Dupee identifies and develops comprehensive mitigation strategies addressing program integrity risks for all of CMS' programs, provides oversight of Medicare Part C and Part D plans and the Federally Facilitated Exchanges, and implements CMS’ Comprehensive Medicaid Integrity Plan. Prior to her current role at CPI, Ms. Dupee worked on such initiatives as the improper payment rate measurement for the Medicare fee-for-service program, Open Payments, and the Healthcare Fraud Prevention Partnership. Ms. Dupee also completed a Congressional detail with the House Committee on Ways and Means, responsible for a portfolio of Medicare fee-for-service and program integrity issues. Ms. Dupee has a Bachelor of Science Degree in Nursing from the University of Wisconsin, a Master of Science in Nursing and a Master of Business Administration from Johns Hopkins University, and a Juris Doctor Degree with a Health Law Certificate from the University of Maryland.
Developing A Payment Integrity Program From The Ground Up
- Developing a Payment Integrity Program from the ground up for a brand new Medicare Advantage Health Plan
- Covering both the opportunities and the challenges of building and effectively managing PI programs that prevent, avoid, or recover billing errors, payment errors and other party liability errors
- Listing of suggestions/ advice from our success, and lessons learned

Monique Pierce
Monique is a Strategic Executive Healthcare Leader with proven ability to develop solutions and maximize the benefits of Payment Integrity programs. She is known for having excellent domain knowledge and being driven, high performing, and having a deep dedication to recruiting and developing top talent.
Monique started her Payment Integrity career at Oxford HealthPlans in the COB and Subrogation Department after spending time in Payment Policy. When United Healthcare acquired many health plans in the early 2000s like Oxford, Monique was tagged as part of the Optum team to integrate the processes and people into the COB systems that she had built at Oxford. She led systems development, quality, reporting, operations, vendor management and was responsible for creating innovative proactive programs that more than doubled savings to $1.4B in three years.
Monique developed a successful program that reduced interest expense on late claims for UHC, assisted a communication company to develop COB tools and assisted in strategic system projects before joining SCIO Health Analytics in 2014 to develop new products - specifically prepayment programs.
In 2015 she became the product owner of SCIOMine, the company’s internal audit application and managed the roadmap. Monique also owned
strategic direction for operational metrics and reporting including executive scorecards. Monique was promoted to VP of Business Opportunities and Client Engagement where she improved Audit Recovery TAT by 39% and reduced client implementations TAT by 11% and the Level of Effort by 18% while increasing the count of implementation projects by 126%.
In 2020 Monique joined Devoted Health, a startup company with the goal of building the first ever integrated Payment Integrity Program. The company has one system, great data, and a great mission; to change health care by treating every member as if they are family.
In her spare time, Monique volunteers her time in the community on the Board of Directors of SCARE NH and works in her family business LARP Portal with her husband Rick.
Claims Audit – The Indiana Jones of Payment Integrity?
- How does Claim Audit fit into the overall savings goals from PI?
- Archaeology amongst savings drivers? High $ treasures?
- Claim Audit Digs & Research – driving process improvement, not just savings.
- Do underpayments matter?
- How to keep finding treasure:
- Partnering with other departments as a true “Partner” not an “Auditor.”
- It will all be in a museum (creating reference materials).

Tom Martin
DOWNLOAD YOUR COPY OF THE AGENDA
REGISTRATION
- Monday, October 30, 2023 to Thursday, May 23, 2024Healthcare Payers and ProvidersCOMPLIMENTARY PASSAn organization that determine service prices, collect payments, and handle claimsA legal entity, or sub-set of a legal entity, which may contract for the provision of health care
Headline
AMS Intelligent Analytics
Website: http://www.amspredict.com/
Advanced Medical Strategies (AMS) is the premier provider of payment integrity, risk management, and business intelligence solutions to identify and address excessive claims, prevent and recoup overpayments, and effectively manage the risks associated with high-cost claimants and group health underwriting.
Platinum Partner
Rialtic
Website: https://www.rialtic.io/
Rialtic is a modern healthcare technology platform focused on payment accuracy. Built by a team of seasoned industry veterans, Rialtic addresses the most important areas of the payment process. Payment policies are highly configurable and customizable: insurers can edit or build their own bespoke policies, while providers can analyze potential reimbursement levels. Robust analytics features across claims, lines of business, payments, and policies provides insightful business intelligence to users. By continuously sourcing, ingesting, and structuring healthcare payment policy documents and data, customers can confidently make up-to-date decisions. Keeping security and compliance top of mind, Rialtic empowers healthcare organizations to work off the same platform with rigorous security controls, a standard in enterprise software.
GOLD PARTNER
4L Data Intelligence
Website: https://4ldata.com/
4L Data Intelligence™ uses the patented power of Integr8 AI™ to find, fight and prevent fraud, waste, and abuse fast with the revolutionary provider-centric FWA approach. Integr8 AI technology, coupled with our continuously credentialed provider database, detects FWA you can’t see with claim data-centric approaches, solving a challenge every payment integrity platform has today.
The 4L FWA Prevention™ solution rapidly detects and prevents FWA at five points across the claims management workflow including pre pre-payment, pre-payment and post-payment positions. At each point, Integr8 AI dynamically and continuously detects provider behaviors, relationships, and outlier status without the limitations of rules-based and claim data-centric solutions. In short, it enables you to see what providers are doing individually, in relationship with all other providers, and in relationship to all other claims on each-and-every claim submitted.
4L FWA Prevention pre-payment and post-payment detection and prevention results are delivered in four distinct categories. These are:
- Provider Integrity Edits
- Adaptive Claims Edits
- Provider Behavior Analysis
- Provider Schemes Analysis.
For fraud and SIU teams, Integr8 AI detects fraud and collusion schemes you can’t see now, or can’t see fast enough, with claim-centric approaches. Our suite of tools automates continuous near real-time SIU-in-a-box detection and documentation so you can Find, Fight and Prevent Fraud Fast™.
Ceris Health
Website: https://www.ceris.com/
CERIS has 30 years of prepay and post pay claim review and repricing experience with a 97% client retention rate. Our solutions are deep, consistent, and defensible reviews, which make CERIS the partner of choice for health plans, Medicare and Medicaid plans, and third-party administrators. CERIS’ longstanding review services and clinical expertise offer incremental value and are grounded in a sincere dedication to our valued partners. CERIS' mission is to continue to grow and deliver long term Payment Integrity services for our partners and to help them save.
CGI
Website: https://www.cgi.com/us/en-us
Founded in 1976, CGI is among the largest IT and business consulting services firms in the world. We are insights-driven and outcomes-based to help accelerate returns on your investments. Across hundreds of locations worldwide, we provide comprehensive, scalable and sustainable IT and business consulting services that are informed globally and delivered locally.
Healthcare Fraud Shield
Website: https://www.hcfraudshield.com/
Healthcare Fraud Shield specializes in fraud, waste, abuse, and error detection and payment integrity for healthcare payers nationally by efficiently stopping claims prior to payment using utilizing post-payment advanced analytics and artificial intelligence insights. We save health plans millions annually incremental to existing pre-payment processes using our unique and proven approach. HCFSPlatform™ offers the combination of targeted rules, artificial intelligence, shared analytics across multiple payers resulting in higher ROI (up to 20:1) compared to other vendors. HCFSPlatform™ software was developed by industry leading healthcare subject matter experts and is a component of over 60+ clients’ including 7 of the 10 largest commercial insurers in the US. Our client satisfaction rating is exceptional with a net promoter score of 84 and client retention rate over 95%. HCFSPlatform™ – is a fully integrated platform consisting of PreShield (prepayment), AIShield (AI), PostShield (post-payment), RxShield (pharmacy analytics), Shared Analytics, QueryShield (ad hoc query and reporting tool), CaseShield (case management), HCFSAudit, and medical record retrieval.
MedReview
Website: https://www.medreview.us/
Headquartered in the financial district of New York City and serving all U.S. states and territories, MedReview has been a leading provider of payment integrity, utilization management and quality surveillance services for more than 40 years. A physician-led organization with a passion for ensuring that health care claims fairly represent the care provided, MedReview provides timely independent hospital billing audits and clinical validation reviews on behalf of health plans, government agencies and Taft-Hartley organizations, saving millions of dollars for its clients each year.
Speakers' Dinner Host
Nokomis
Website: https://nokomishealth.com/
Nokomis was founded in 2013 by our current CEO Rich Henriksen to ensure Claim Accountability and make a difference in the healthcare system.
We are still privately owned and therefore only have to answer to our customers - that’s the way we like it.
Through 35 years in healthcare, Rich and his team compiled their deep and broad knowledge to build Nokomis and its proprietary technology, ClaimWise™. This unique technology finds patterns in claim data to identify claims for further review, regardless of dollar amount. Combined, ClaimWise™ and the Nokomis team intelligently select claims for review, finding errors even in claims that look fine at face value.
EXHIBITOR
6 Degrees Health
Website: https://www.6degreeshealth.com/
6 Degrees Health is on a mission to reduce the cost of healthcare. We take a service-first approach to our Clean Claim Reviews to ensure accuracy in billing and fair payments. Using our extensive cost containment experience, clinical expertise, and next-generation, purpose-built software, we deliver remarkable savings for health plans. Our proprietary review process leverages CMS and other industry standard guidelines to evaluate every line item and identify billing errors and inconsistencies.
These pre-pay clinical reviews are completed by our team of highly trained and experienced registered nurses to ensure each billed line item is appropriate for reimbursement. This detailed review removes erroneous line items and verifies billing accuracy. Our comprehensive process manages claims during the review stage, as well as through payment and appeals resolution. Our white glove service on appeals allows us to maintain an uphold rate of 97 %, so your savings are secure.
Alivia Analytics
Website: https://www.aliviaanalytics.com/
Power & Modernization for the Healthcare Payment Continuum. Alivia’s revolutionary, AI-enabled Analytics Platform offers payer modules that include Claims Editing integrated with pre- and post-pay adjudication workflows to stop erroneous billing; FWA Finder™ that generates 100x more fraud and improper payment leads and unique FWA scenarios; Alivia Case Manager that opens 10x more fraud cases and decrease pre-case cost by 50-90% in our platform, or yours; VBC Insights for 1000+ Episodes of Care that shortens negotiation durations and lowers costs; and MCO Insights to support the encounter management submission process for Managed Care Organizations. We also address Payment Integrity challenges through Tech-Enabled Services performing FWA Investigations, Clinical Reviews, Recovery Audits, and ESRD Premium Protection. Alivia’s 2024 acquisition of SourcEdge added unique expertise to optimize core systems with Data Consolidation, De-Indentification, and Claims Systems IT. Our customers are commercial health plans to Medicare Advantage and Medicaid Managed Care Plans. Alivia delivers actionable insights, visible ROI, speed, and accuracy leveraging technology, medical, clinical, and law enforcement experience. HITRUST Certified.
Apixio
Website: https://www.apixio.com/
Apixio, formerly ClaimLogiq, is the Connected Care Platform at the intersection of health plans and providers. Our AI technology and flexible services power risk adjustment, payment integrity, and care delivery programs using centralized patient health profiles, data-driven insights, and seamless workflows. By combining ClaimLogiq and the Apixio technology ecosystem, healthcare organizations can streamline operations, ensure accurate payment, and uncover critical patient insights—building a resilient foundation for success as the industry moves toward value-based reimbursement models. Visit apixio.com to learn more.
CoventBridge
Website: https://coventbridge.com/
CoventBridge Group has more than 25 years of experience in the identification, prevention and investigation of fraud, waste, and abuse for our customers across the healthcare, insurance, financial and government markets with a proven track record of implementing and managing the largest programs in the industry. CoventBridge is the partner of choice supporting:
- 8 of the top 10 commercial carriers in the U.S.
- 7 of the top 10 personal line carriers in the U.S.
- Centers for Medicare and Medicaid Services as the Program Integrity contractor investigating Healthcare FWA
- One of the largest government agencies providing a national network of undercover investigators
CoventBridge offers the following services and more via its 500+ investigators:
Program Management
• Audits & Assessments
• Compliance Assessment
• Medicare & Medicaid FWA
• On-site Audits
• Vendor Management
Document Retrieval & Analysis
• Medical Record Retrieval
• Medical Record Review & Coding (RN)
• Investigative Medical Record Review
• Medical & Healthcare Canvassing
Investigative Services
• Healthcare FWA Investigations
• Investigative Reports
• Clinical Surveillance
• Law Enforcement Referrals
• Alive and Well Checks
Staff Augmentation
• Data Analysts
• Investigators
• Nurse Reviewers
• RN Consultants
Data In Formation
Website: https://liberty-source.com/
Liberty Source PBC is a U.S.-based provider of technology-enabled human-in-the-loop data services that help companies realize maximum value from their Artificial Intelligence, Machine Learning, and Business Intelligence investments. Through its flagship DataInFormation brand, the company provides image annotation, data labeling, computer vision calibration, NLP validation, training data curation, prompt engineering, model monitoring / data lineage evaluations, and related data optimization services.
100% of facilities, operations and workforce are US-based to provide the highest level of information security; to minimize time zone issues; and to eliminate challenges arising from different cultural interpretations of data. 80+% of the staff are veterans or members of military families.
Liberty Source has deep domain expertise in a wide range of industry verticals. Extensive capabilities and a nimble culture are key differentiators that enable the company to fulfil even the most rigorous client requirements.
DRG Claims Management
Website: https://www.drgclaims.com/
DRG Claims Management is an accuracy and integrity solutions firm, auditing claims for DRG and Clinical Validation, Cost Outliers, Readmissions, Short-Stay/OBS, and Skilled Nursing Facilities. Health Care Organizations partner with us to increase payment integrity savings and to improve claim payment performance. Our audits are completed on a Prepay, Post-payment or Hybrid basis.
HealthPlan Data Solutions, Inc.
Website: https://hds-rx.com/
Bridging the divide between payers and PBMs with payment integrity solutions. HDS is a software solutions company that leverages leading-edge technology paired with pharmacy expertise to help payers proactively manage the performance of their PBM. Our PBM-agnostic approach leverages over 500 proprietary claim scanning algorithms that are custom coded to identify, monitor, and fix claims adjudication issues ranging from plan design implementation errors to compliance and regulatory errors. Our unique approach to payment integrity is more than PBM auditing and places all the information at the payers fingertips. Your pharmacy data. One platform. Complete visibility.
Machinify
Website: https://www.machinify.com/
Machinify is transforming healthcare administration with AI. At the core of Machinify is an AI cloud platform that digests and unifies policies, guidelines, and data transforming healthcare administration. Machinify's platform and services power revolutionary applications that interoperate for seamless execution across the healthcare claims lifecycle:
- Machinify Audit: End-to-end system utilizing GenAI and large language models (LLMs) to perform automated coding validation of complex claims.
- Machinify Pay: Software that enforces coding and payment policies against claims and prices claims accurately.
Penstock Group
Website: https://www.penstockgroup.com/
Penstock is a service partner and SaaS builder for forward-thinking health plans and providers, empowering recovery, audit and regulatory teams to get accuracy right from the start—when it matters most. Our mission is to create lasting systemic change that removes wasted spend from our healthcare system, returning dollars to payers, lowering the cost of care and improving access for all.
Penstock is powered by industry veterans who are some of the most sought-after payment integrity and regulatory experts in the industry. Our business model is rooted in transparency and the drive to reinstate true integrity in payment integrity—even if it defies traditional business sense.
Our audit workflow SaaS platform, ClearBridge gives health plans the tools and insights they need to identify overpayments, correct them and implement their own edits with ease, ensuring correct payments and mitigating future discrepancies.
When you partner with Penstock, you reclaim time and control with an end-to-end partnership that beautifully and seamlessly connects human and machine intelligence—to prevent recurring issues at the source.
Trend Health Partners
Website: https://www.trendhealthpartners.com/
Combining the strengths of Trend, PrecisionGX and Advent, Trend Health Partners emerges as a pioneer in healthcare financial optimization, delivering unparalleled payment integrity and revenue cycle expertise since 2010. As a trusted partner for providers and payers, we are dedicated to elevating payment accuracy and reducing administrative costs through our innovative, tech-enabled solutions. Our robust platform and clinical team operate as a seamless extensions of a provider’s business office, resolving credit balances, overturning denials and managing claims with precision and efficiency.
At Trend Health Partners, we personalize our approach to meet the unique needs of each client, ensuring the recovery and saving of billions of dollars while supporting their long-term financial objectives. We are committed to accelerating accurate reimbursements and enhancing revenue integrity by merging clinical insights, best practices, and cutting-edge technology.
Our mission extends beyond financials; we foster collaboration and transparent communication across the healthcare spectrum, offering a suite of services that drive significant value for all stakeholders. With a legacy of industry leadership, Trend Health Partners stands at the forefront of healthcare innovation. Together, we are setting new benchmarks for collaboration, transparency and integrity in the healthcare industry.
Accredited by:
AAPC
Website: https://www.aapc.com/medical-coding-education/
Health care professionals are obligated to stay current in their profession. This includes continuing education in their respective discipline as well as keeping up with the latest medical coding updates, compliance rules, and government regulations. AAPC supports its members to maintain a distinctive edge in their health care career by providing a wide variety of topics and subject matter delivered live or on demand, in classrooms or over the web.
PARTNER WITH US
Based on your objectives, we can create bespoke packages designed specifically for you – from presenting your expertise on the main stage, to hosting a private dinner. You can partner with us showcase your brand and make valuable new connections. Opportunities predominantly lie in 3 main categories: Thought Leadership, Branding & Networking.
To discuss your objectives and partnership opportunities please contact Harry Ludbrook, Sales Director [email protected]
Interested in a media partnership?
We'd love to hear from you and how we can support one another to connect with the industry. Contact Jodie Purser, Marketing Manager, [email protected]
PARTNER WITH US
Based on your objectives, we can create bespoke packages designed specifically for you. Opportunities predominantly lie in 3 main categories: Thought Leadership, Branding, and Networking.
Interested in a media partnership?
We'd love to hear from you and how we can support one another to connect with the industry. Contact [email protected]
Delivering scalable and flexible solutions which ensure accuracy and integrity of claims
The Healthcare Payments and Revenue Integrity Congress is the only summit focused on addressing healthcare waste and ensuring that claims are paid correctly, reflecting current healthcare needs. You will join key decision-makers, within health insurers and providers, who are responsible for payment and revenue integrity, value-based payment, and networking relations.
At a time when both payers and providers are evaluating and streamlining internal payment and revenue integrity processes, this networking conference has been established to breakdown silos, by promoting discussion between clinical, coding, revenue cycle and payment departments to facilitate the development of efficient, value-based healthcare systems.
Venue
MILLENNIUM MAXWELL HOUSE HOTEL 2025 Rosa L Parks Blvd, Nashville, TN 37228
 We're excited to welcome you face-to-face in Nashville at Millenium Maxwell House Hotel for the Healthcare Payment & Revenue Integrity Summit!
We're excited to welcome you face-to-face in Nashville at Millenium Maxwell House Hotel for the Healthcare Payment & Revenue Integrity Summit!
If you're looking for accomodation, you can book at a discount here.

MEDIA KIT

For more information on webinars, roundtables, content marketing packages, interviews and marketing solutions opportunities, download the Media Kit.
If you have any questions, please contact Harry Ludbrook, Sales Director, [email protected].
About Kisaco Research
Kisaco Research produces, designs and hosts B2B industry conferences, exhibitions and communities – focused on a specialized selection of topic areas.
Meet industry peers that will help build a career-changing network for life.
Learn from the mistakes of your peers as much as their successes—ambitious industry stalwarts who are happy to share not just what has made them successful so far but also their plans for future proofing their companies.
Note down the inspired insight that will form the foundation for future strategies and roadmaps, both at our events and through our online communities.
Invest both in your company growth and your own personal development by signing up to one of our events and get started.
We'd love to hear from you.
Contact us at +44 (0)20 3696 2920 and email [email protected], or let us know what subject area you're interested in below.